What does the word placebo mean?
Does the placebo effect involve actual health benefits or just imagined benefits?
Is placebo “mind over body” or “all in your head”? Is it unethical to provide a client with placebo treatments? And what about nocebos?
In this article, I’ll answer these questions and discuss some fascinating research by Fabrizio Benedetti and colleagues.
After reading this you will have a better understanding of placebo, and you might even stop using the word, because it’s fairly ambiguous, and often a poor explanation for why a treatment helps someone to move better or feel better.
What Exactly Is The Placebo Effect?
Placebo is a confusing term because it means different things when used in different contexts.*
For purposes of this article, it has the following meaning: A placebo is a treatment that reduces symptoms only because the patient expects a benefit, not because the treatment itself has any effect.
For example, a sugar pill can be a placebo that will improve a headache only if the person taking the pill expects that it will provide benefits. But if the person does not expect benefit, it’s no longer a placebo, and does nothing.
The placebo effect is the physiological process by which expectations about a treatment cause changes in the brain that initiate an improvement in symptoms. These changes are real, not imagined.
In other words, if someone experiences a real placebo effect, they are not just imagining some improvement – there are objective and measurable changes in their physiology to prove it.
The nocebo effect is basically the opposite: It causes negative changes in symptoms (e.g. more pain and reduced function) when there is an expectation that an otherwise harmless stimulus will cause harm.
Clearing Up Mind-Body Confusions
Placebo is often described in terms of a “mind-body connection.”
This suggests it involves some sort of mysterious process, or that we need to radically change our way of thinking to understand it.
But in fact, the connection between abstract thought and events in the body should be intuitive and trivially obvious. If I form an intention to reach for a cup, my hand actually reaches for the cup! If I think there is an intruder in my house, my heart will beat faster and I may begin to sweat. If I spend my life worrying, I increase my risk of headaches and heart attacks.
So we already know that thoughts affect the body.

In other words, the placebo effect does not involve anything magical. It is one of many ways that our cognition affects our physiology. But it is a very interesting and clinically relevant phenomenon because it reveals the mechanisms by which our thoughts and expectations affect the way we move and feel.
What Can The Placebo Effect Do?
Placebos can cause changes in pain level, motor control, muscle tension, strength, endurance, energy level, depression, immune response, heart rate, and glucose level.
They can even make you drunk!
But placebos don’t help with everything. They won’t cure cancer, make you taller, and they probably don’t help with asthma. Placebo effects are often significant. In the case of pain, they can change self-reported pain scores two points on a ten-point scale.
The rest of the article will focus on placebo effects as they relate to pain.
How Does The Placebo Effect Work To Reduce Pain?
The easiest way to understand how a placebo can affect pain is by considering the purpose that pain serves.
Pain is an unpleasant feeling designed to protect you from perceived threat to the body.
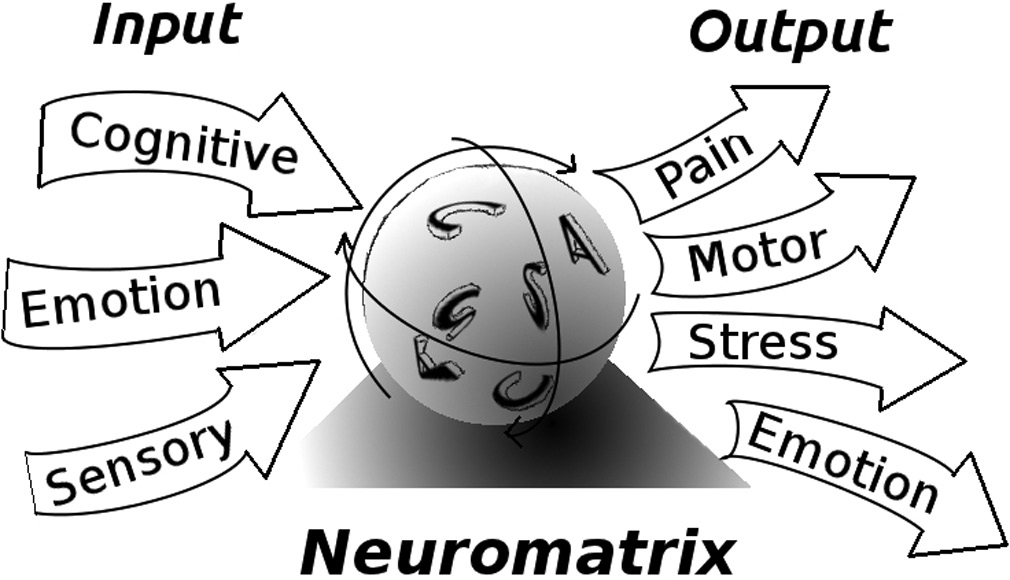
Placebos alter the perception of threat and therefore the pain. And that works as follows. The brain is always in the process of unconsciously analyzing threats to the body, based on all the information it can gather. This information comes from a wide variety of sources, including sensory data from the body, visual data from the eyes, memories, opinions, and, importantly, information that is provided by medical authorities.
Thus, when a doctor tells you something about some condition in your body, or the medicine intended to treat it, this becomes part of the evidence base from which your brain unconsciously determines whether pain is needed to protect you from that condition. Put another way, your opinions about the effects of a placebo treatment become one of many cognitive inputs that modify the output of pain.
The research of Benedetti and others has identified three different patterns of mental processes that create the placebo effect: (1) expectations of benefit; (2) reduction of anxiety; and (3) learning through association. Let’s look at each in turn and the associated physiological processes.
Expectation Of Reward
One way placebos work is by creating an expectation of benefit, which activates the reward system of the brain.
The reward system motivates us to engage in behaviors that maximize the spread of our genes, such as eating food, having sex, getting money, and basically doing all the things that humans are generally very motivated to do. The reward system involves release of dopamine. For example, when you experience the reward of getting social approval, you get a little hit of dopamine, which makes you want to do it again.
It’s like a built-in dog trainer. Facebook likes, good boy!

Here’s how we know the reward system is involved in placebos that reduce pain.
The placebo effect is greater in people who get more dopamine release when rewarded. It’s also stronger in people who experience more rewards from receiving money. Further, nocebo effects are associated with dopamine reduction. Also, the improvement in motor control that a Parkinson’s patient experiences after a placebo is correlated with release of dopamine in parts of the brain related to motor control.
So how exactly does activation of the reward system reduce pain?
One mechanism for reward-based analgesia is descending inhibition of nociception. This involves the brain sending opioids or other drug-like substances down the spinal cord to block nociceptive signals (danger signals that often result in pain) from getting to the brain. David Butler calls this system the “drug cabinet in the brain.”
How do we know this system is involved in the painkilling effects of placebo? Because when you give people drugs that block the operation of this system, they don’t get any placebo effect from expecting a reward. Here’s a cool example to illustrate.
Researchers put tourniquets on the arms of subjects and asked them to squeeze a ball for as long as possible, to the limits of their pain tolerance. One group was told the procedure would benefit their muscles, and the other was told nothing. Not surprisingly, the group expecting benefit was able to tolerate the pain longer. Here’s the cool part: increased pain tolerance from an expectation of benefit was completely eliminated by drugs which prevented activation of the descending inhibition system.
So we know that descending modulation is involved in placebo effects related to expectation of reward. I think it probably plays a role in the pain relief we often see from exercise, foam rolling or trigger point work. Interestingly, many common chronic pain conditions such as fibromyalgia, chronic fatigue, and IBS are characterized by the relative inefficiency of the descending inhibitory systems. We should expect that these groups are less likely to experience placebo effects based on the expectation of reward.
Anxiety Reduction
Another mechanism by which placebos work is reduction of anxiety. Anxiety basically means the state of expecting a future threat. (It can be distinguished from fear, which is the perception of a current threat.)

Research shows that placebos can reduce anxiety, which tends to decrease pain.
Nocebos do the opposite – they increase anxiety and pain. For example, in one study, researchers told volunteers that a very low-intensity electrical stimulus would be painful. And so it was, even though it shouldn’t have hurt much at all.
Again, the effects are real not imagined – researchers measured the increase in anxiety and pain not just by subjective report, but objective measures of activity in relevant brain areas. Further evidence that nocebos have real physiological effects comes from research showing that it can be eliminated by drugs that reduce anxiety, such as benzodiazepine and diazepam.
In other words, if you can’t be made anxious by false suggestions that something will hurt you, it won’t hurt any more than it should. Anxiety also works to antagonize the dopamine and opioid networks that cause placebo pain relief.
Learning
If you consistently experience pain relief right after a certain stimulus, you will learn to associate the stimulus with reduced pain.
For example, if you regularly take aspirin to help with a headache, you will begin to associate the appearance of the pill with feeling better. If someone then gives you a fake aspirin that looks like the real one, you will get a much better placebo effect than without the prior conditioning.
Thus, past experience can make you “expect” benefit from a particular stimulus, even if that expectation is purely unconscious and based on past associations.

These associations can be “unlearned” as well.
If you ring a bell for a Pavlovian dog, he will salivate – but if you keep ringing and never bring dinner, at some point he will figure it out and stop drooling.
And if you keep taking that same placebo aspirin without its active ingredient, it will eventually lose any learned placebo effect.
Here are some interesting experiments that demonstrate how learning through association can create placebo effects.
Rats who learn to associate a favored liquid with receiving an immunosuppressive drug will experience immune suppression after drinking the liquid, even if the drug is removed. Similar results have been obtained in humans. A tasty beverage will improve runny noses in people with allergies if it is first consistently paired with an antihistamine.
Unconscious learning can also create placebo effects in the endocrine system. A fake insulin injection can lower blood sugar after a conditioning process with actual insulin.
This is all very interesting to be sure, but why should a manual or movement therapist care?
We are (hopefully) not in the business of giving our clients drugs during treatment to cause them to associate our care with pain relief.
Here’s why we should care: This research gives insight into what is probably a major player in pain relief related to movement therapy – “unlearning” negative associations between movement and pain. These associations can arise after an injury, and remain to cause a big fat nocebo effect even after the injury heals. Imagine you injure your back, and then experience nociception and pain whenever you forward bend into full lumbar flexion. You will start to consciously or unconsciously associate this movement with pain, and you will gradually learn to expect pain when you do the movement.
After a while, the back injury heals but the association remains.
Forward bends are now a nocebo that can create pain even without the “active ingredient” of nociception. How do we stop this nocebo effect? By breaking the learned association between forward bending and pain.
If you repeat the forward bend enough, especially in ways that are slow, novel and non-threatening, your brain will eventually realize that the “active ingredient” of nociception is no longer present. You will start to unlearn the association between movement and pain, and eventually recover full pain free flexion.
But what if you don’t fully go through this unlearning process?
Maybe the injury heals and nociception is gone, but you avoid the movement completely because you’re too scared to revisit it. The nocebo effect remains because you never break the association between pain and movement. This is perhaps one of the reasons why fear of movement (kinesophobia) is a good predictor of when acute injuries will develop into chronic pain. I think the one of the main ways that movement therapy can help us get rid of chronic pain is to progress slowly and carefully into movements which we expect either consciously or unconsciously to cause pain.
For an amazing and dramatic example of this process, check out this video by Peter O’Sullivan.
Conclusion
The science of placebo is very interesting and informative.
It is not unreasonable to suppose that a good degree of the success seen in movement-based therapies is through placebo-like effects, or through getting rid of nocebos.
But I think the word placebo can be confusing. It refers to a wide variety of different phenomena that have different effects through different mechanisms. Some placebo effects work through anxiety reduction, others through activation of the reward system, and others through descending inhibition of nociception. The common thread is they are all created by cognitive inputs – information that changes what the patient expects or believes about their health.
And this relates to another problem with the word placebo – it suggests that treatments which work through changes in client expectation are somehow inert, or ineffective, or not meaningful, or unethical, or even a scam. Of course this may very well be the case when the treatment is a sugar pill, or based on pseudoscience or quackery. In these instances, the clients’ expectations and beliefs are changed because they are deceived, and this is in most cases unethical.
But what if a treatment works primarily through changes in belief and expectation, but in a way that changes those beliefs to be more accurate? Consider the following scenarios, all of which might be described as involving placebo effects, but none of which involve deception:
- a client is given accurate information about the poor correlation between back pain and objective MRI findings. This lowers his anxiety and pain.
- a client is shown through passive and active movement that it is possible for her to bend forward without pain if she does so in a different manner. This reduces her anxiety, makes her expect benefit from therapy, and this reduces her pain.
- a client receives compassionate and empathetic treatment from a caring therapist. This lowers his anxiety, makes him expect benefit, and thereby reduces his pain.
- a client has had many past experiences with massage causing pain relief, and this learned association contributes to further pain relief from massage.
Are these all placebo effects?
It is true that they all work in large part by changing the client’s beliefs. But that was the whole point of the treatment in the first place! So there should be no suggestion that the treatments are inert, ineffective or deceptive. Using the word placebo in these cases can be stigmatizing and confusing.
I prefer to look at it this way: pain results from perception of threat, and it can be treated by providing the client as much good news as possible about the threat in question. Does this present an ethical issue? Only when that good news is built from lies and not the truth. Fortunately, I think there are many optimistic truths that clients can learn from therapists through touch, movement, and conversation.
*Another meaning for placebo is used in the context of research trying to determine whether some treatment is effective. This meaning includes various reasons the data reflects that a subject feels better after a treatment, such as spontaneous remission of the disease, data error, or regression to the mean. In this context, if my headache was about to get better in the next hour, and I took a pill right before that, my improvement would be attributed to “placebo.” Yet another meaning for placebo is something that causes a subject to think that they feel better, or to report that they feel better, even when there haven’t been any real objective changes in their symptoms.
from Beauty Salon, Spa, Massage https://themtdc.com/the-science-of-placebo/
No comments:
Post a Comment